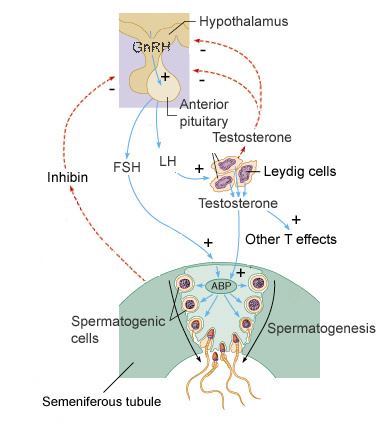
The male testis consists of tightly packed seminiferous tubules. Within these tubules the formation of sperm (spermatogenesis) occurs. Leydig cells between the tubules secrete the male steroid, Testosterone (T) and Sertoli cells secrete a peptide hormone, Inhibin. Sertoli cells also feed the maturing sperm. Secretion of T at puberty initiates spermatogenesis, induces development of the male accessory organs, stimulates protein synthesis, induces male secondary sexual characteristics, and increases sex drive. Testicular function, including the action of the Leydig and Sertoli cells, is stimulated by two tropic hormones, Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) from the anterior pituitary. Release of these tropic hormones is under hypothalamic control through the pulsatile release of the neurohormone, Gonadotropin Releasing Hormone (GnRH). T and Inhibin inhibit the hypothalamus and/or the pituitary glands.
Although more complex, ovarian function is also controlled by FSH and LH. FSH stimulates folliclar growth around an ovum which over the next 14 days enlarges in size. The follicle cells feed the ovum and release a female steroid, Estrogen (E), which feedbacks positively on the hypothalamus and pituitary. Estrogen also stimulates uterine development. On Day 14, a surge in LH occurs which results in ovulation. The remnant follicle cells form the corpus luteum, which begins to secrete a second steroid, Progesterone (P). P inhibits uterine contraction while encouraging development of the uterine mucosa for possible implantation of the egg. P also inhibits development of additional ova. If fertilization fails to occur, the corpus luteum and egg deteriorate. In the absence of inhibitory P, a new ovarian cycle starts. Should fertilization of the egg occur, the diploid zygote begins to divide while in the oviduct and eventually implants as a blastocyst in the uterine wall. Once implanted, a unique blend of fetal and maternal tissues, called the placenta, quickly develops to supply the developing fetus with oxygen and nutrients while removing waste products. The placenta is also an endocrine organ and very early on begins to produce Human Chorionic Gonadotropin (HCG), a peptide hormone. HCG stimulates the corpus luteum to continue secreting P. Later, the placenta synthesizes its own P. Estrogen (mammary gland development), Placental Lactogen (mammary gland development and increased blood glucose and fatty acids), and Parathyroid Hormone Related Peptide (encourages Ca++ delivery) are also produced by the placenta. At the end of pregnancy, the peptide hormone, Relaxin, is released that softens the cervix in preparation for birth.
Excerpted and adapted from: Reproductive System